Manual lymphatic drainage (MLD), an often-overlooked aspect of maternal health, plays a pivotal role in optimizing breastfeeding outcomes. The lymphatic system, integral to immune function and fluid homeostasis, intersects with lactation physiology in ways that are increasingly recognised in breastfeeding care [1,2]. Emerging research suggests that targeted lymphatic interventions could significantly alleviate common breastfeeding challenges such as engorgement, mastitis, and lymphatic congestion, ultimately enhancing both maternal comfort and breastfeeding success [1,3,4,5].
Despite the well-documented benefits of breastfeeding, including its critical role in neonatal immune development, the physical demands on lactating mothers remain substantial. Issues such as breast engorgement and inflammation not only contribute to maternal discomfort but also pose risks to the continuity and success of breastfeeding [4]. Traditional management strategies, including the use of heat packs, cabbage leaves, and analgesics, while somewhat effective, often neglect the lymphatic system’s contribution to these conditions [6]. This oversight may limit the efficacy of treatments designed to support lactating mothers, particularly in the early postpartum period when breastfeeding is most vulnerable to disruption [4].
We spoke to Kristina Chase, a specialist in Lymphatic Drainage Massage and an Australian Lymphology Association accredited Lymphoedema Practitioner. We discussed with Chase the potential of MLD as a therapeutic approach in breastfeeding management. By drawing upon recent studies and expert insights, we will examine how lymphatic health directly impacts lactation and propose a paradigm shift in breastfeeding support practices that integrate lymphatic care. Through this lens, we aim to advance the discussion on maternal health and offer evidence-based recommendations for clinical practice.
Definition and Mechanism
Lymphatic drainage is a critical physiological process essential for maintaining fluid homeostasis, supporting immune function, and facilitating the clearance of cellular debris. The lymphatic system, comprising a network of vessels and nodes, operates in tandem with the circulatory system to transport lymph—a clear fluid enriched with immune cells—throughout the body. Unlike the circulatory system, the movement of lymph is driven by muscle contractions and the intrinsic contractility of lymphatic vessels moving lymph via one-way valves towards the heart, rather than by a central pump like the heart [7].
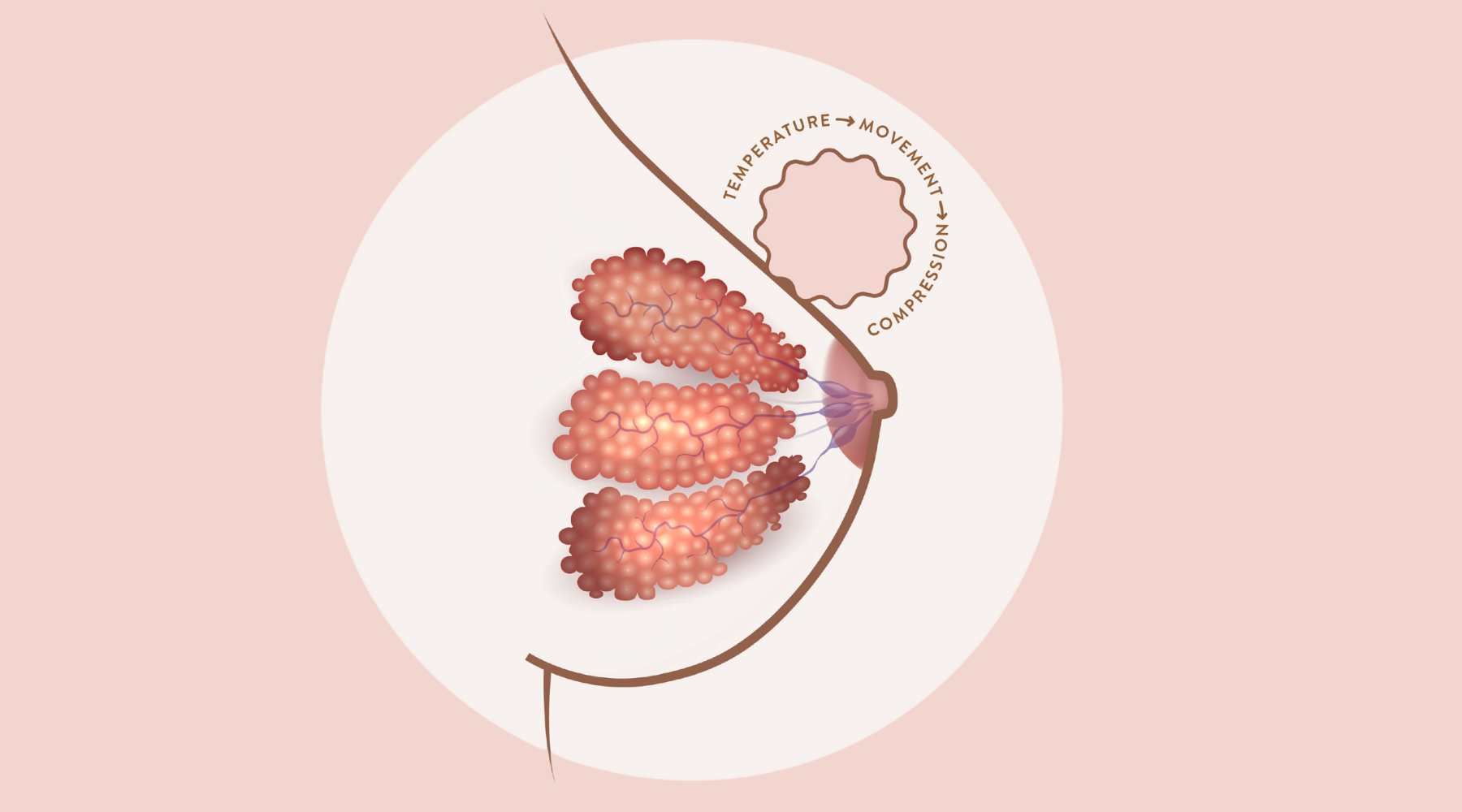
In the context of lactation, the lymphatic system in the breast is crucial for managing the increased fluid exchange that occurs during milk production. Chase explains the intricate network of lymphatic vessels within the breast tissue helps prevent fluid accumulation and inflammation, common issues during breastfeeding. However, when lymphatic flow is impeded—due to factors such as engorgement or inflammation—fluid can accumulate, leading to congestion and an increased risk of conditions like mastitis [1,3].
Chase describes the lymphatic system as the body's "detoxification system," facilitating the removal of cellular debris, toxins, and pathogens. By mobilising this waste through lymphatic vessels toward the nodes, where immune cells such as macrophages neutralise harmful elements, the system ensures that the body maintains optimal fluid balance and immune defense. In cases of breast engorgement, the lymphatic system can become congested due to inflammation, impeding fluid flow and exacerbating inflammatory responses. Thus, maintaining effective lymphatic flow is crucial not only for addressing acute issues like engorgement but also as a preventative measure to support overall breast health during lactation.
Chase stresses this integrated approach to understanding lymphatic drainage highlights its potential as a vital component in the management of breastfeeding-related conditions, offering significant benefits for both immediate symptom relief and long-term maternal well-being.

Current Research and Evidence
The efficacy of MLD in managing lactation-related complications such as breast engorgement, plugged ducts, and mastitis has been increasingly supported by recent research. A comparative study on MLD and Kinesio Taping (KT) found that the MLD group experienced significant reductions in both pain and breast engorgement across all post-intervention days. Notably, milk volume increased more substantially in the MLD group compared to both the KT and control groups, underscoring MLD's superior efficacy in enhancing milk production during lactation [3].
Research by Witt et al. [4] on Therapeutic Breast Massage in Lactation (TBML) further underscores the importance of MLD. The study revealed that TBML, which incorporates gentle MLD through massage towards the axilla combined with hand expression, provides immediate and significant relief from pain associated with engorgement, plugged ducts, and mastitis. Additionally, mothers reported that TBML was beneficial not only immediately but also for managing future episodes of mastitis and plugged ducts, indicating its potential for long-term benefits.
Another study focusing on the integration of MLD with Thai Traditional Massage (TTM) in postpartum mothers demonstrated that while the combined therapy did not significantly differ from standard care alone in terms of breast milk volume and pain reduction, the mothers who received MLD plus TTM expressed high satisfaction with the intervention. This satisfaction was linked to perceptions of reduced pain and improved milk production, suggesting that MLD, especially when combined with other therapeutic methods, could offer broader benefits that extend beyond immediate symptom relief [5]
These studies collectively suggest that MLD is a valuable tool in lactation management, providing substantial benefits for both immediate relief and long-term maternal well-being. However, further research is warranted to optimize these techniques, explore their full range of applications, and establish comprehensive guidelines for their use in clinical practice.
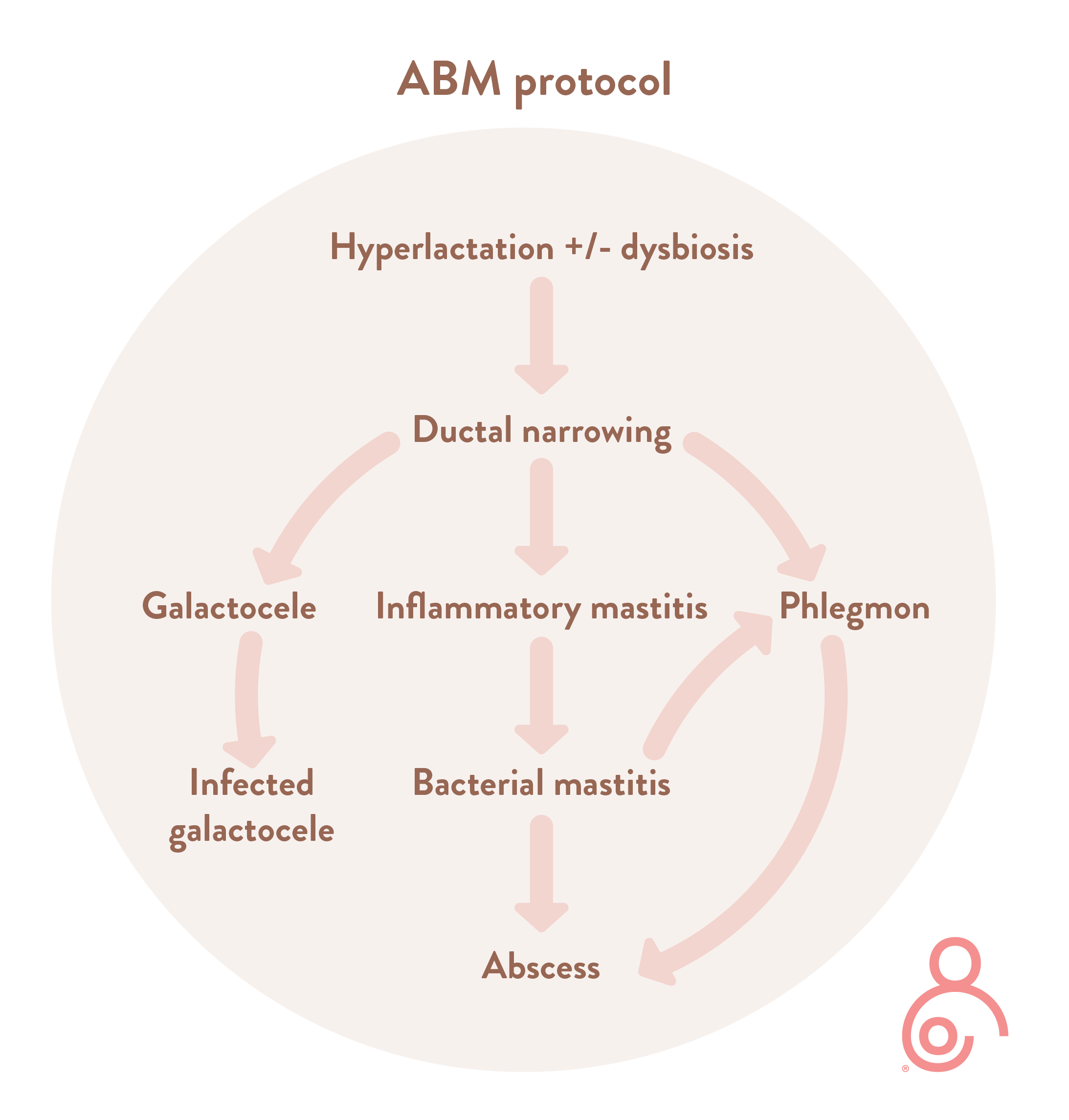
Chase discusses the role of heat in lymphatic drainage, particularly in the context of breastfeeding. She clarifies that while heat can be highly effective in promoting vasodilation and facilitating the movement of fluids, thereby easing lymphatic congestion, its application should be based on the individual's condition. Specifically, in cases of severe inflammation or discomfort associated with breast inflammation, heat may exacerbate symptoms. As outlined in the Academy of Breastfeeding Medicine’s Protocol 36 (ABM Protocol 36) on the mastitis spectrum, the use of heat should be guided primarily by the mother’s comfort. While it can offer maternal comfort in some scenarios, heat or warmth should be tailored to the severity of the inflammation and the specific needs of the patient. Applying a cold press can also be beneficial especially to help reduce inflammation and pain following a breastfeed. Chase expresses an individualised approach is key suggesting them to try both warmth and cooling to obtain the most relief.
Integration into Breastfeeding Care Practices
To maximise the benefits of lymphatic drainage, it is imperative that healthcare providers incorporate these techniques into standard breastfeeding support protocols, particularly during the hospital stay when initial lactation issues are most likely to arise. The early initiation of lymphatic drainage can provide a proactive approach to managing potential complications, thereby improving long-term breastfeeding outcomes. As Chase notes, "Lymphatic drainage techniques can benefit all breastfeeding women by maintaining healthy fluid movement and reducing the risk of inflammation-related issues." Alongside MLD, techniques such as thoracic breathing and dry brushing can also further support the lymphatic system. ABM Protocol 36 on the mastitis spectrum emphasises the necessity of employing light, sweeping motions characteristic of MLD, as opposed to deep tissue massage, which can exacerbate inflammation or damage delicate breast tissue. Clinical findings further support that excessive pressure may impede rather than facilitate lymphatic flow, counteracting the therapeutic intentions of the procedure. It is also crucial to acknowledge the contraindications and potential risks associated with MLD. Chase explains that in cases of active infection or abscess formation MLD should be used cautiously and in conjunction with appropriate medical treatment to avoid the risk of spreading infection. Additionally, the application of heat in conjunction with MLD should be moderated to suit the needs of the individual as highlighted in ABM Protocol 36; while warmth can aid in fluid movement and provide maternal comfort, excessive heat may exacerbate inflammation, particularly in cases of significant inflammation. These considerations underscore the need for a nuanced application of lymphatic drainage techniques within the broader spectrum of breastfeeding support.
As Chase notes, "in cases of breast engorgement, the lymphatic system becomes congested due to inflammation, impeding the flow of lymphatic fluid. This stagnation exacerbates inflammation, making lymphatic drainage essential to relieve congestion, promote fluid movement, and reduce both pain and inflammation in breastfeeding mothers,".
By Kate Bird, IBCLC
References
- Moura SO, Borges LCC, Carneiro TMA, Silva APSD, Araújo RM, Ferreira GLC, et al. Therapeutic Ultrasound Alone and Associated with Lymphatic Drainage in Women with Breast Engorgement: A Clinical Trial. Breastfeed Med. 2023 Nov;18(11):881-887. doi: 10.1089/bfm.2022.0269. PMID: 37971376.
- Bolman M, Saju L, Oganesyan K, Kondrashova T, Witt AM. Recapturing the art of therapeutic breast massage during breastfeeding. J Hum Lact. 2013 Aug;29(3):328-31.
- Doğan H, Eroğlu S, Akbayrak T. Comparison of the effect of Kinesio taping and manual lymphatic drainage on breast engorgement in postpartum women: A randomized-controlled trial. Breastfeed Med. 2021;16(1):82–92. doi:10.1089/bfm.2020.0115.
- Witt AM, Bolman M, Kredit S, et al. Therapeutic breast massage in lactation for the management of engorgement, plugged ducts, and mastitis. J Hum Lact. 2016;32:123–131.
- Sritas S, et al. Evaluating the safety and efficacy of manual lymphatic drainage with Thai traditional massage on breast milk volume, breast pain and engorgement in Post-Cesarean Mothers of preterm infants: A randomized controlled trial. Open Public Health J. 2023;16(1). doi:10.2174/0118749445267207230919070638.
- Pevzner M, Dahan A. Mastitis While Breastfeeding: Prevention, the Importance of Proper Treatment, and Potential Complications. J Clin Med. 2020 Jul 22;9(8):2328. doi: 10.3390/jcm9082328. PMID: 32707832; PMCID: PMC7465810.
- Breslin JW, Yang Y, Scallan JP, Sweat RS, Adderley SP, Murfee WL. Lymphatic Vessel Network Structure and Physiology. Compr Physiol. 2018 Dec 13;9(1):207-299. doi: 10.1002/cphy.c180015. PMID: 30549020; PMCID: PMC6459625.