Low milk supply is one of the most common concerns for breastfeeding mothers and a significant cause of early cessation of breastfeeding. Approximately 35% of mothers report concerns about insufficient milk production, leading them to introduce formula or discontinue breastfeeding earlier than intended [1]. Given the critical role that breastfeeding plays in infant health and development—offering immune protection, promoting optimal growth, and reducing the risk of chronic diseases—addressing low milk supply is essential [2].
We spoke with Kate Visser, endorsed midwife, registered nurse and IBCLC. Visser spoke to the synthesis of breastmilk and the role that breast massage can play as a non-invasive, effective solution to addressing low milk supply. Among the various techniques to support breastfeeding, breast massage has emerged as a non-invasive, natural approach that not only enhances milk production but also fosters maternal familiarity with breast health [2]. Although underutilised in clinical practice, breast massage, when integrated into a comprehensive breastfeeding support plan, offers immediate and long-term benefits for milk production and maternal confidence. This article examines the physiological mechanisms underpinning breast massage and its impact on lactation, emphasising its role in hormonal regulation and lymphatic drainage.
Synthesis of milk and hormonal regulation
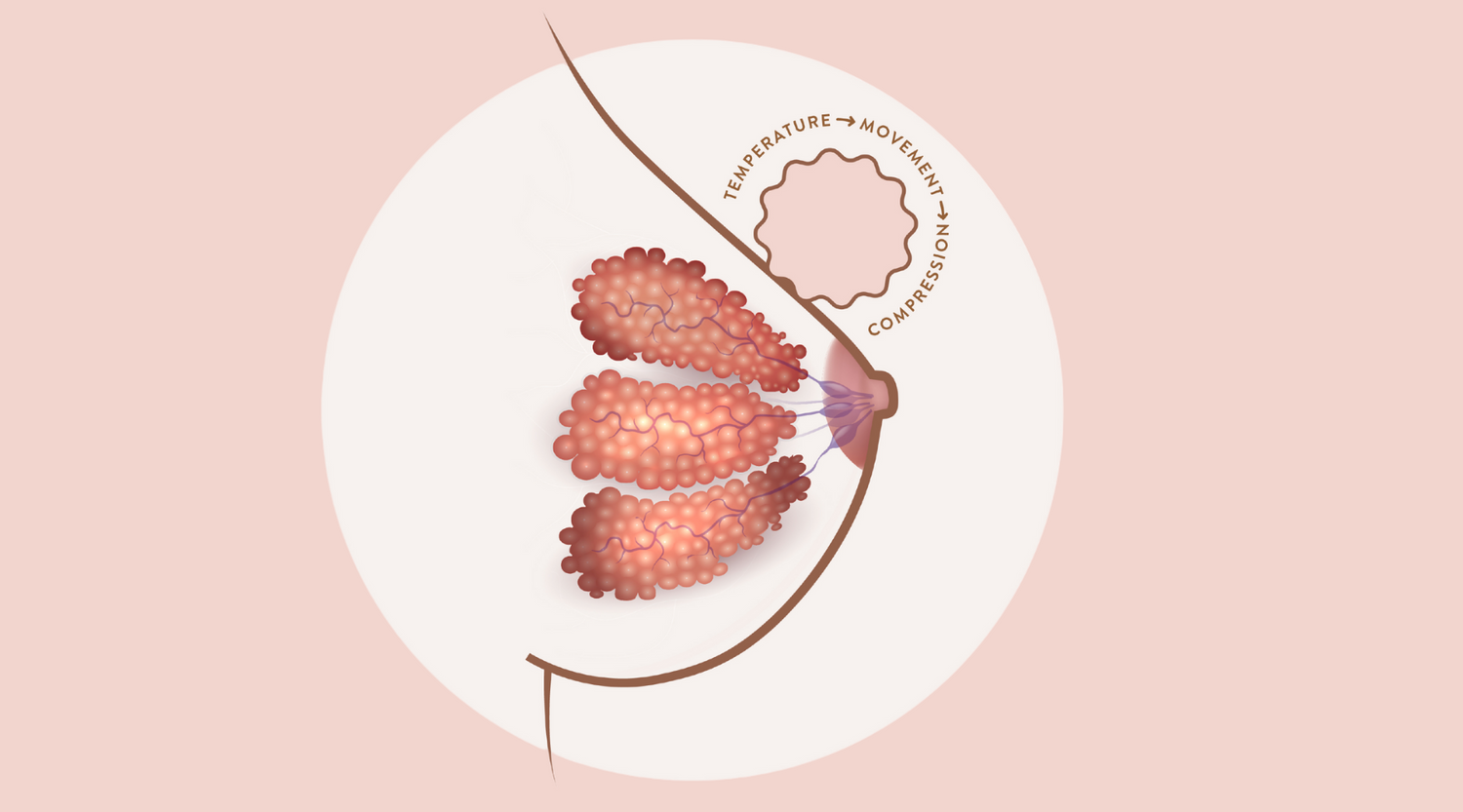
Visser explained milk synthesis is a complex physiological process regulated by key hormones, primarily prolactin and oxytocin, which play critical roles in lactation. Prolactin, secreted by the anterior pituitary gland in response to nipple stimulation, is responsible for stimulating the mammary alveolar cells to produce and secrete milk. The amount of prolactin released is directly proportional to the frequency and intensity of breastfeeding or manual stimulation, making consistent breast stimulation essential for sustaining milk production [2].
The let-down reflex, triggered by oxytocin, involves the contraction of the myoepithelial cells surrounding the alveoli in the mammary glands. Oxytocin is released in response to tactile stimulation of the breast, causing the milk stored in the alveoli to be ejected through the ducts and into the nipple, where the infant can access it. This reflex is crucial for ensuring that milk is available to the infant during feeding. Additionally, oxytocin release is associated with emotional bonding between mother and child, further reinforcing the physiological and psychological dimensions of breastfeeding.
Understanding low milk supply
Low milk supply can result from a range of underlying factors [1]. Visser shares “there may be issues related to hormones- we know that oxytocin and prolactin are essential hormones for breastfeeding, but many other hormones can come into play. Insulin resistance, elevated progesterone levels from retained placental fragments, raised oestrogen levels from ovulation or the combined oral contraceptive pill, elevated testosterone for some women with polycystic ovarian syndrome, even raised cortisol from sustained high stress can all contribute to a low milk supply.” These disruptions interfere with the finely tuned supply-demand mechanism that regulates milk production. Additionally, insufficient stimulation of the breast, whether due to infrequent feeding or ineffective milk removal, sends negative feedback to the body, further reducing milk output. Over time, this cycle of reduced stimulation and lower milk production can lead to early weaning, depriving the infant of the well-documented benefits of breastfeeding, such as immune system enhancement, optimal nutrition, and psychosocial bonding [2].
Concerns about low milk supply are widespread, often driving mothers to supplement with formula. While supplementation may appear to offer a short-term solution, it can undermine breastfeeding by reducing the frequency and effectiveness of breast stimulation, which is essential for maintaining milk production [3]. Visser, alongside the research, expressed that mothers who perceive their milk supply as inadequate are more likely to discontinue breastfeeding prematurely, which can have profound long-term consequences for both maternal and infant health [4].
Breast massage as a natural approach to managing low milk supply
Breast massage offers a non-invasive method to enhance milk production by improving blood circulation, promoting lymphatic drainage, and stimulating the milk ducts. In a clinical setting, Divya et al. (2016) observed that breast massage significantly increased the volume of expressed milk among mothers of infants in neonatal intensive care units (NICUs) [5]. Visser explains “Breast massage is a very underappreciated intervention that can improve a low milk supply in two ways- hormonal and milk release.” Breast massage is its role in stimulating the release of prolactin and oxytocin, two hormones essential for successful lactation. Research has shown that manual breast stimulation through massage can increase prolactin levels, particularly in the early postpartum period when milk supply is being established [1]. Similarly, breast massage enhances oxytocin release, improving milk ejection and flow [5]. By optimising this hormonal environment, breast massage plays a crucial role in sustaining milk production over time [6].
Breast massage not only supports milk supply but also enhances maternal familiarity with breast anatomy and overall breast health. The tactile connection established through massage fosters greater confidence in managing breastfeeding and promotes maternal self-efficacy [5]. “Prior to breastfeeding, breasts are tied to this innately sexual part of our body. Besides a self breast check, most women have never handled their breasts before” explains Visser. Further sharing that women who are more comfortable in handling their breasts are often more confident, open to intervention or support when needed and experience greater breastfeeding outcomes.
Breast massage is most effective when used in conjunction with other lactation-supporting methods, such as frequent breastfeeding, ensuring proper latch techniques, and the use of breast pumps. Combining massage with hand expression or pumping results in more complete breast drainage, which is essential for stimulating ongoing milk production [3]. In this way, breast massage functions as a valuable component of a comprehensive breastfeeding support strategy, offering both immediate improvements in milk flow and long-term benefits for milk supply sustainability.
Beyond its hormonal benefits, breast massage supports lymphatic drainage, an important process in preventing engorgement and blocked ducts—two conditions that can severely impede milk flow [5]. Enhanced circulation within the breast tissue ensures that milk is released more effectively, and that essential nutrients reach the mammary glands, supporting sustained milk production over time [(5]). The integration of breast massage into lactation care not only optimises the physiological conditions for successful breastfeeding but also reduces the risk of complications that can disrupt milk flow.
Underutilisation of breast massage in lactation support
Despite its proven effectiveness, breast massage remains underutilised in clinical practice. Kate notes in her experience breast massage is under utilised by both mothers and professionals, “even when information is presented, it may seem too simple, as if it’s too good to be true”. Further research indicates that many healthcare providers lack adequate training in teaching proper breast massage techniques, and mothers are often unaware of its benefits [3]. Cultural barriers and discomfort with manual breast manipulation further limit the adoption of this cost-effective and accessible intervention [4]. Given the significant benefits associated with breast massage, its underutilisation represents a missed opportunity in the provision of holistic breastfeeding support.
Integrating breast massage education into antenatal classes and postpartum care has the potential to significantly improve breastfeeding outcomes [5]. Healthcare providers play a critical role in promoting breast massage as part of a comprehensive breastfeeding support strategy. By educating mothers on this technique, healthcare professionals can empower women to manage common breastfeeding challenges, such as low milk supply and engorgement, more effectively [3]. The simplicity of breast massage and its accessibility make it an ideal intervention for a wide range of settings, particularly in areas where access to lactation consultants or other specialised care may be limited.
As a non-invasive, low-cost intervention, breast massage can be easily practised by mothers [6] Visser shares “massage may be performed consciously by the mother in a variety of ways, such as stroking towards the nipple or with a Lactamo ball”. This accessibility makes it a particularly valuable tool for managing low milk supply in settings where access to medical interventions or professional lactation support is limited [6]. Moreover, breast massage offers psychological benefits by reducing maternal anxiety and increasing confidence in breastfeeding [4]. The practice empowers mothers to take an active role in addressing breastfeeding challenges, which in turn enhances their overall breastfeeding experience.
Breast massage represents a valuable and underutilised tool in the management of low milk supply, offering a range of physiological and psychological benefits. Through its ability to enhance circulation, stimulate the release of essential lactation hormones, and promote lymphatic drainage, breast massage plays a critical role in both the immediate improvement of milk flow and the long-term maintenance of milk production. When integrated with other breastfeeding support techniques, breast massage serves as a key component of a comprehensive lactation strategy.
The current underutilisation of breast massage highlights the need for increased education and training among healthcare providers and mothers. Incorporating breast massage into standard lactation care has the potential to improve breastfeeding outcomes, reduce the incidence of breastfeeding-related complications, and empower mothers to take control of their breastfeeding journey. For these reasons, healthcare providers should actively promote breast massage as part of their breastfeeding support protocols, ensuring that mothers are equipped with the tools they need to succeed in their breastfeeding goals.
References
- Anderson L, Kynoch K, Kildea S, Lee N. Effectiveness of breast massage for the treatment of women with breastfeeding problems: a systematic review. JBI Database System Rev Implement Rep. 2019 Aug;17(8):1668-1694. doi: 10.11124/JBISRIR-2017-003932. PMID: 31135656.
- Kent JC, Prime DK, Garbin CP. Principles for maintaining or increasing breast milk production. J Obstet Gynecol Neonatal Nurs. 2012 Jan;41(1):114-21.
- Divya A, Viswanath L, Philip A. Effectiveness of Breast Massage on Expression of Breast Milk among Mothers of Neonates Admitted in Neonatal Intensive Care Unit. J South Asian Feder Obst Gynae 2016;8(1):1-4.
- Kent JC, Prime DK, Garbin CP. Principles for maintaining or increasing breast milk production. J Obstet Gynecol Neonatal Nurs. 2012 Jan;41(1):114-21.
- Divya A, Viswanath L, Philip A. Effectiveness of Breast Massage on Expression of Breast Milk among Mothers of Neonates Admitted in Neonatal Intensive Care Unit. J South Asian Feder Obst Gynae 2016;8(1):1-4.
- Kent JC, Prime DK, Garbin CP. Principles for maintaining or increasing breast milk production. J Obstet Gynecol Neonatal Nurs. 2012 Jan;41(1):114-21.