Mastitis is a common lactation complication, affecting ~25% of women in the first 26 weeks postpartum.1
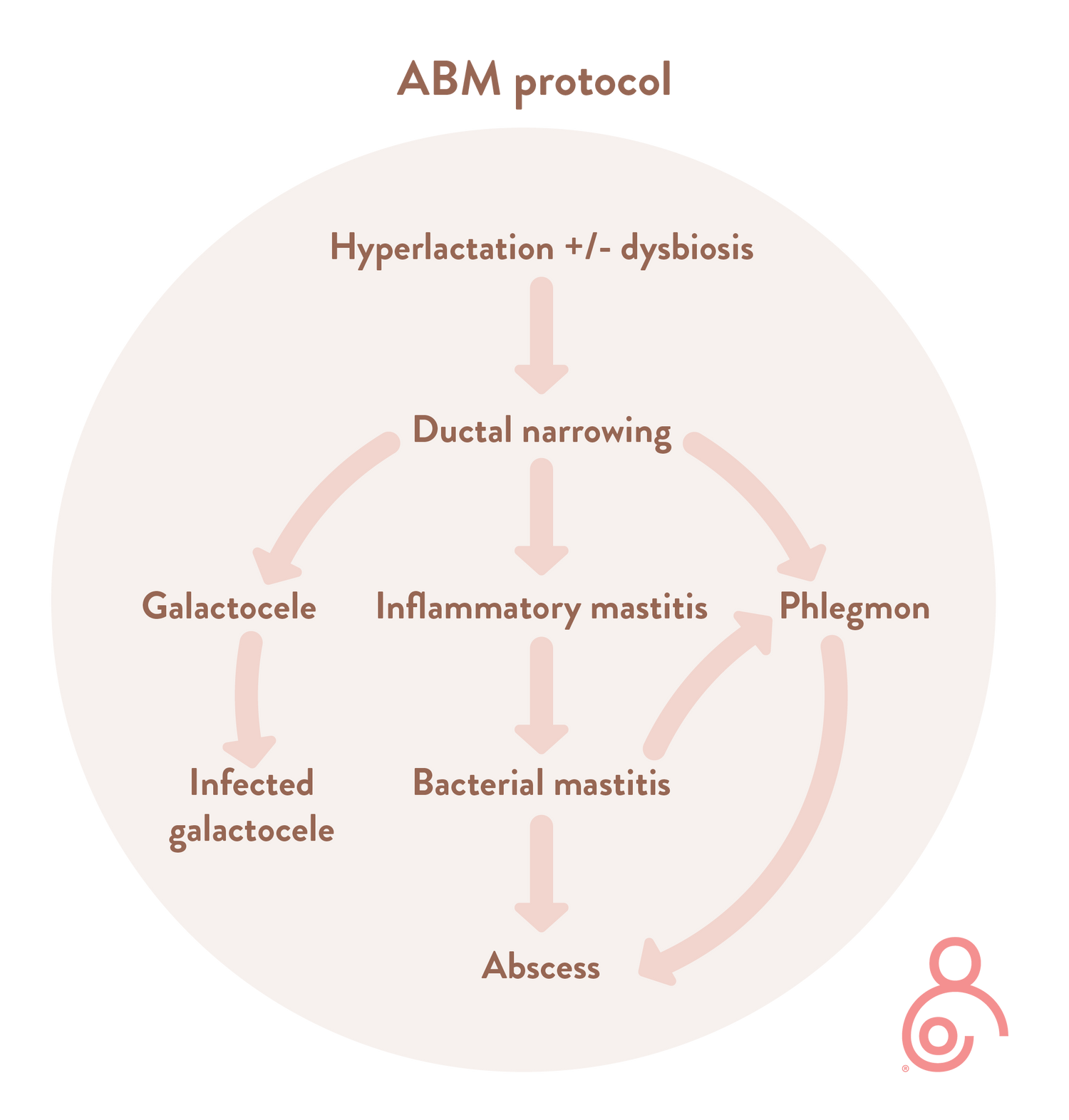
Historically, mastitis has been considered as pathology presenting in the lactating breast alone2, but newer scientific evidence shows that it encompasses a range of conditions resulting from ductal inflammation and stromal oedema.3
Papers published by Dr Douglas on breast inflammation have resulted in a shift in our understanding of the causes of mastitis, and therefore a need to change the assessment and management moving forward.4,5
Douglas’ analysis proposed a mechanobiological model of breast inflammation in which very high intra-alveolar and intra-ductal pressures are hypothesised. It is proposed that this pressure puts strain on, or ruptures the tight junctions between lactocytes and ductal epithelial cells, triggering inflammatory cascades and capillary dilation. The increase in stromal tension leads to pressure on lactiferous ducts, resulting in a worsening of intraluminal backpressure. Rising leucocyte and epithelial cell counts in the milk and alterations in the milk microbiome are signs that the mammary immune system is recruiting mechanisms to downregulate inflammatory feedback loops leading to potential pain and oedema which can then worsen the ductal pressure.4,5
The key for prevention and treatment of breast inflammation is to avoid excessively high intra-alveolar and intra-ductal pressures, which prevents a critical mass of mechanical strain and rupture of the tight junctions between lactocytes and ductal epithelial cells.
Pressure in the ductal system may occur for a number of reasons:
- Engorgement/oedema
- Hyperlactation
- Milk stasis
- Underlying anatomical features e.g. dead-end ducts, previous surgery
- External compression from clothing or massage
ABM protocol

The revised ABM protocol has created change in how we need to think about and manage mastitis. It is now important to disseminate the new information to women needing this information through adequate support and education.
Therapeutic Breast Massage and Lymphatic Drainage
The revised guidelines from the protocol introduce therapeutic breast massage and lymphatic drainage as innovative strategies for managing lactation-related discomforts. The guidelines advocate for therapeutic breast massage as a means to facilitate lymphatic drainage and alleviate congestion within the breast tissue, while advising against the use of intense deep tissue massage or vibrating devices that could potentially cause harm. Whilst this highlights that some commercially available breastfeeding products are not suitable, it’s interesting to see how Lactamo directly aligns with the protocol: Lactamo allows women to avoid deep tissue massage whilst facilitating breast massage and lymphatic drainage as recommended by the protocol.
Despite the growing popularity of breast massage and lymphatic drainage among health professionals, many women express uncertainty regarding the appropriate intensity and pressure for effective massage. Again, the benefits of Lactamo are clear: Lactamo facilitates this process in an easy to use way, enabling mums to proactively and reactively address these problems with ease and more confidence.
Lactamo emerges as a novel solution, diverging from traditional massage devices by being tailor-made for the lactating breast. Its design incorporates a jelly-like center that ensures the applied pressure remains within therapeutic bounds, minimizing the risk of microvascular damage. Lactamo's unique composition is engineered to complement the mechanical and elastic characteristics of breast tissue, which vary significantly from the softer adipose tissue at 0.5 kPa to the firmer skin tissue at 3,000 kPa. The device's exterior softness mirrors the gentle yet effective touch required for therapeutic massage.
The protocol also addresses the contentious use of heat in breast massage, acknowledging that while theoretically heat could exacerbate inflammation, some women may still find it comforting. Lactamo accommodates this preference by allowing for its use at a comfortable warmth or at room temperature, ensuring versatility in its application for therapeutic purposes. Additionally, Lactamo offers the advantage of being cooled, providing not only comfort but also aiding in reducing inflammation between feeding sessions, further underscoring its utility and innovation in lactation support.
Prevention and management
The revised ABM protocol looks at general strategies for the management of mastitis spectrum disorders, as well as condition-specific interventions.3
Overall principles are categorised as follows:


For condition-specific recommendations, please refer to the full protocol.
We know the benefits of therapeutic breast massage, and there is much research available to support its use in many breastfeeding conditions. However, without adequate training/direction/instructions, the techniques used can often cause more harm than good. The use of gentle massage, using the right combination of three critical components - temperature, movement and compression – has shown to have benefits in many conditions including mastitis.
"Prompt and effective treatment will halt progression in the [mastitis] spectrum."3
This article is written by Kate Barry, RN IBCLC
References
-
Wilson E, Woodd S, Benova L. Incidence of breast milk expression and associated factors in women in the UK: A cross-sectional study. J Hum Lact. 2020;36(4):673-686.
-
Kvist LJ. Toward a clarification of the concept of mastitis as used in empirical studies of breast inflammation during lactation. J Hum Lact. 2010 Feb;26(1):53-9. doi: 10.1177/0890334409349806. PMID: 19910519
-
Mitchell KB, Johnson HM, Rodríguez JM, Eglash A, Scherzinger C, Zakarija-Grkovic I, Cash KW, Berens P, Miller B; Academy of Breastfeeding Medicine. Academy of Breastfeeding Medicine Clinical Protocol #36: The Mastitis Spectrum, Revised 2022. Breastfeed Med. 2022 May;17(5):360-376. doi: 10.1089/bfm.2022.29207.kbm. Erratum in: Breastfeed Med. 2022 Nov;17(11):977-978. doi: 10.1089/bfm.2022.29207.kbm.correx. PMID: 35576513.
-
Douglas P. Re-thinking benign inflammation of the lactating breast: A mechanobiological model. Womens Health (Lond). 2022 Jan-Dec;18:17455065221075907. doi: 10.1177/17455065221075907. PMID: 35156466; PMCID: PMC8848036.