Understanding breast anatomy when you’re trying to breastfeed might help explain some of the changes and challenges many new mamas experience and help overcome some of the more common breastfeeding issues.

Having a baby is a magical time for any new mama. But no one would deny there’s a lot to take in. Between the birth, breastfeeding, recovery, and all those hormones, it can feel overwhelming.
Having a bit of knowledge up our sleeves might help. While many new mamas plan to try breastfeeding, few of us know anything about female breasts, breastfeeding, how our breasts work, or the aids that might help us, such as Lactamo, if we’re having a tough time.
Lactation consultant, registered nurse accredited in neuro protective developmental care, and a busy mama to two beautiful boys, Kyleen Sayer runs her own lactation consultant business, Lactation Connect. Working with women as they navigate their own personal feeding journey, Kyleen is dedicated to helping and educating those who want extra support.
We asked Kyleen to explain the breast anatomy, how we produce milk and why some of the most common breastfeeding challenges occur.
How is the breast structured?
While breasts may appear to be simple in structure, they are in fact made up of several complex components that work together to enable breastmilk production and delivery.
“The female breast anatomy is composed primarily of mammary tissue but also contains milk producing glands – called lobules,” explains Kyleen. “These lobules hold tiny sacs called alveoli, and are linked by a network of thin tubes, also known as ducts. The breast structure also includes nipple, areola, connective tissue, fat, blood and lymphatic vessels, and nerves.” 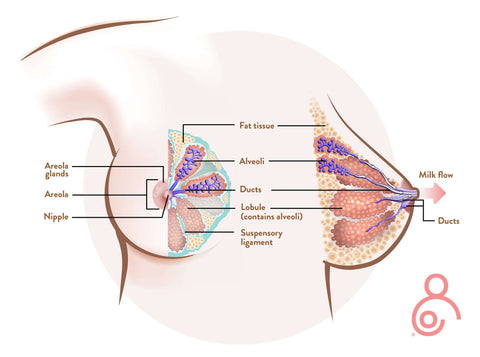
What happens when we breastfeed?
This is where the astounding cleverness of our brains and bodies really kicks in, says Kyleen. “When baby suckles at the breast, the brain receives a signal, causing the hormones prolactin and oxytocin to be released. Prolactin causes the alveoli to begin making milk, while oxytocin causes the muscles around the alveoli to squeeze and move milk out through the ducts. This is also known as the milk ejection reflex, more commonly known as the ‘let down’.”
If that’s all a bit medical, don’t worry. The reality is that your body will be doing all of this amazing work by itself. All a new mama has to do is rest and gaze down at your new baby – science will take care of the technical part!
How and why does breast anatomy change during pregnancy?
From the moment you conceive, a mama’s body starts to change, says Kyleen, who is quick to add that these changes are a normal part of pregnancy.
“Changes in the breasts are due to hormonal fluctuations and can occur as early as one week after conception and continue as you progress throughout, and after, pregnancy.”
Once again, hormones cause the changes, this time estrogen and progesterone. “These hormones prepare the breasts for lactation,” explains Kyleen, who says some of the more common changes can include (but are not limited to):
- tenderness
- discomfort
- enlargement
- darkened nipples and areolae
- veins appear more prominent
- colostrum production.
Can every breast breastfeed?
If all breast anatomy is structured in the same way, is every breast able to breastfeed?
Yes – and no, says Kyleen.
“I hear many women voice concerns over too large or too small breasts, or different shaped nipples. With the right support systems and education in place, ideally before the baby is born, breastfeeding should be possible for the vast majority of women.”
But says Kyleen there are some anatomical and medical exceptions that may have implications for breast milk supply and/or feeding. These include:
- piercings
- breast surgery (including removal and/or repositioning of nipples)
- concerns regarding ‘insufficient glandular tissue’
- trauma
- endocrine or hormonal concerns.
“I would recommend talking to a lactation consultant before birth to flag any concerns to ensure the correct support systems can be put into place.”
Can I help prepare my breasts for breastfeeding?
Pregnant women are encouraged to prepare for birth and yet are rarely given support around how to get ready for breastfeeding. But, is there anything we can do to prepare our bodies?
"There's actually nothing that you need to do to prepare your breasts for breastfeeding, this will occur naturally,” says Kyleen. “Once you are pregnant your physiology takes over and is preparing your body and your breasts.”
“I’ve heard people say they tried to toughen, harden, or roughen their nipples before baby was born, but you certainly don’t need to do that. Trust your body to do its job.”
What new mamas can do to help feel prepared says Kyleen is seek advice and help early on and not wait until the baby arrives.
“So much of the overwhelm I see in new parents would be greatly minimised if the education and information had been provided during pregnancy.”
For any new mama wanting to breastfeed it’s important to know that those precious minutes, hours and days just after baby is born are especially important. Research tells us that the first 60 minutes of a baby’s life, known as ‘the golden hour’ may be crucial in setting up a successful feeding journey. Maintaining skin-to-skin contact with your new baby not only helps to regulate their temperature and prevent distress but can also help baby to breastfeed and bond with mama. Read more here about the golden hour.
What is the most important part of breastfeeding?
Having spent more than a decade helping new mamas on their breastfeeding journey, Kyleen says the one take away she would pass on is very simple.
“I’d say to any new mama, be true to yourself and what you want your feeding journey to look like. Whether that is exclusive direct breastfeeding, some direct breastfeeding with expressed breast milk via pumping, or a combination of other feeding methods with breast milk substitute. There is still a lot of stigma and shame around how we choose to feed our children. So be true to yourself, because we want you to enjoy the experience.”
Every feeding journey is different. If your feeding plan doesn’t play out in the way you’d first hoped, don’t be disheartened. “There should never be any judgement on how a mama chooses to feed their baby,” says Kyleen. “But I want them to know that there is support available, regardless of the way that they choose to feed.”
Where can I find support and help?
Lactation Consultants of Australia and New Zealand can help you find a lactation consultant near you.
Ask your GP, midwife, obstetrician, or healthcare provider to connect you with a lactation consultant locally.
The Australian Breastfeeding Association have many resources available including a 24-hour helpline for new mamas, face-to-face workshops, and online classes.
Read more here: